Experience Healthcare IT with Heart
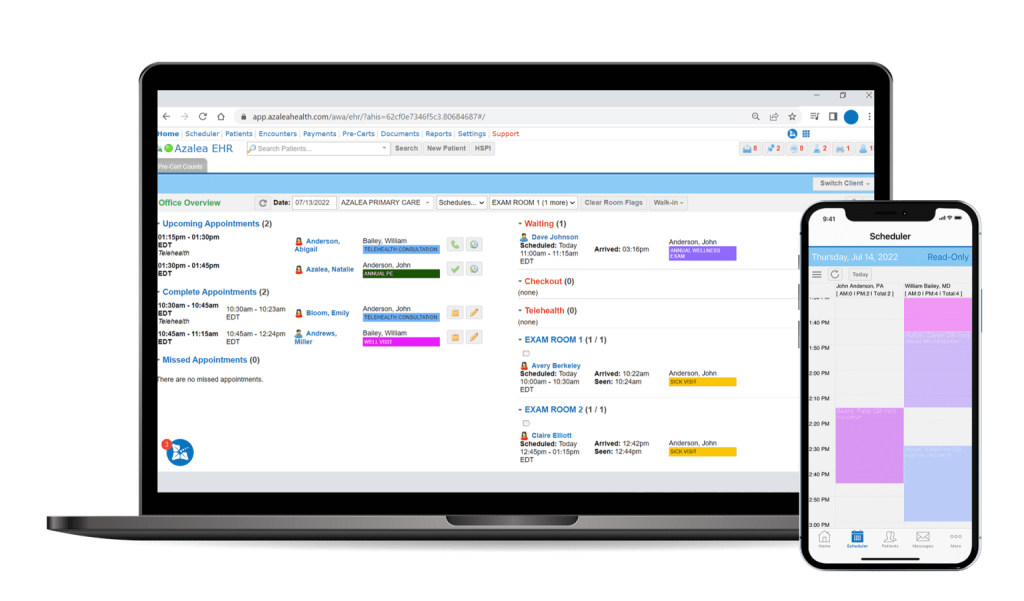
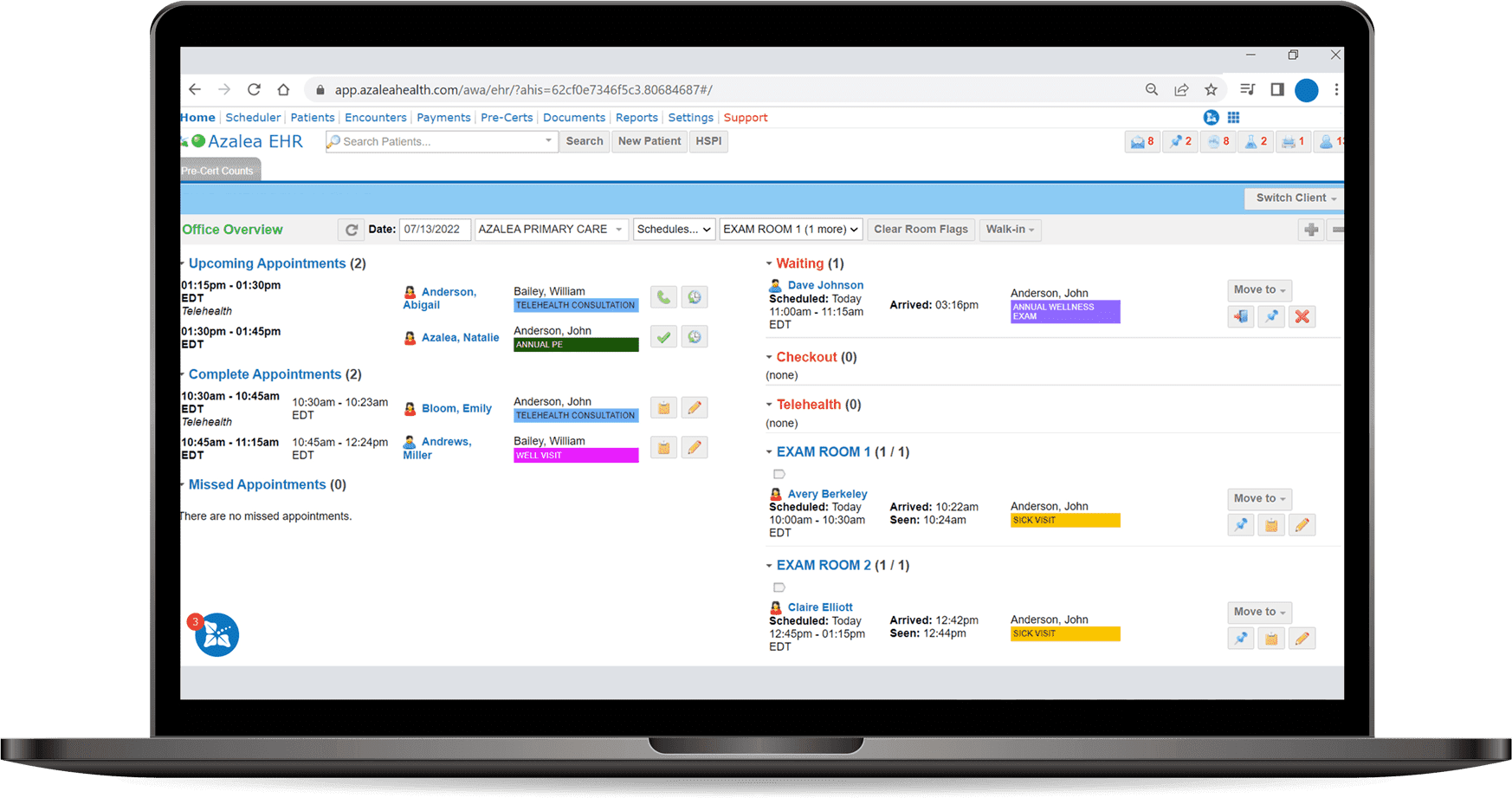
Azalea Health empowers care providers with simplified and seamless technology that boosts your ability to provide care—all while supporting your work-life balance. Learn more about our award-winning cloud-based healthcare software.
A Provider First Platform

Trusted where it
matters most
Rural providers are often the sole health resources for their communities—that’s why our platform was designed, and is trusted, to meet your needs and the needs of your patients.

More than a
platform—a partner
With Azalea Health, we are not just your EHR provider, we are a resource and a partner you can rely on. We’re just a call or click away whenever you need us.

Guided by a
singular vision
The Azalea Health platform is purpose-built to create one record of truth for each patient—enabling providers to be informed and intentional with their care.

Focused on what’s important
We make technology invisible so providers can be more present.

100% cloud-based
Our secure 100% cloud-based platform accelerates the impact of care and future-proofs your hospital or clinic.

Simple and seamless
Our platform streamlines the way care is delivered, enhancing your patient’s experience- while minimizing time spent charting after hours.
Core Offers
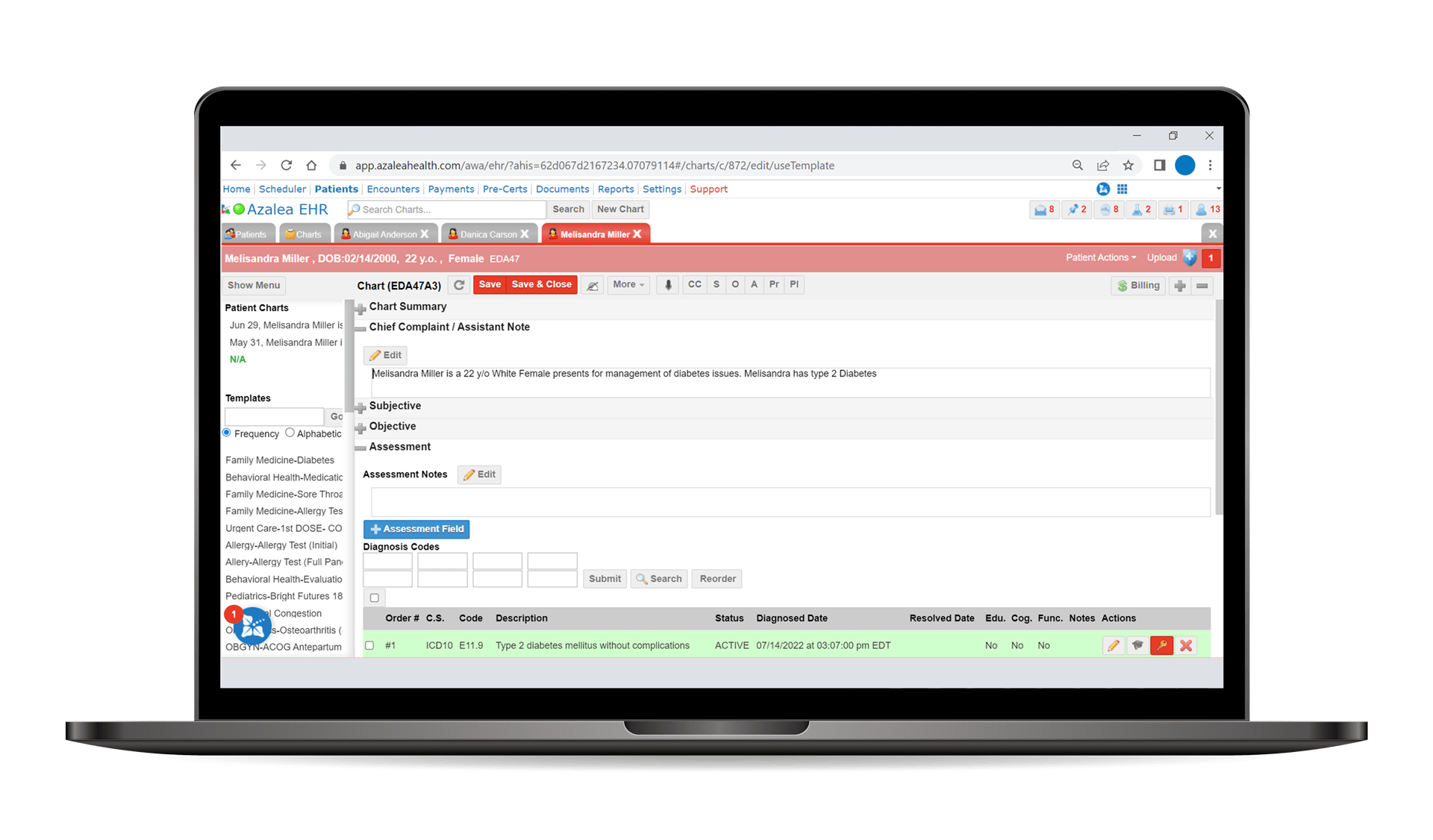
Unify patient data into a single, efficient record of truth that translates across all components of our platform—meaning your team is always in the know when it comes to your patients’ care.
Learn More
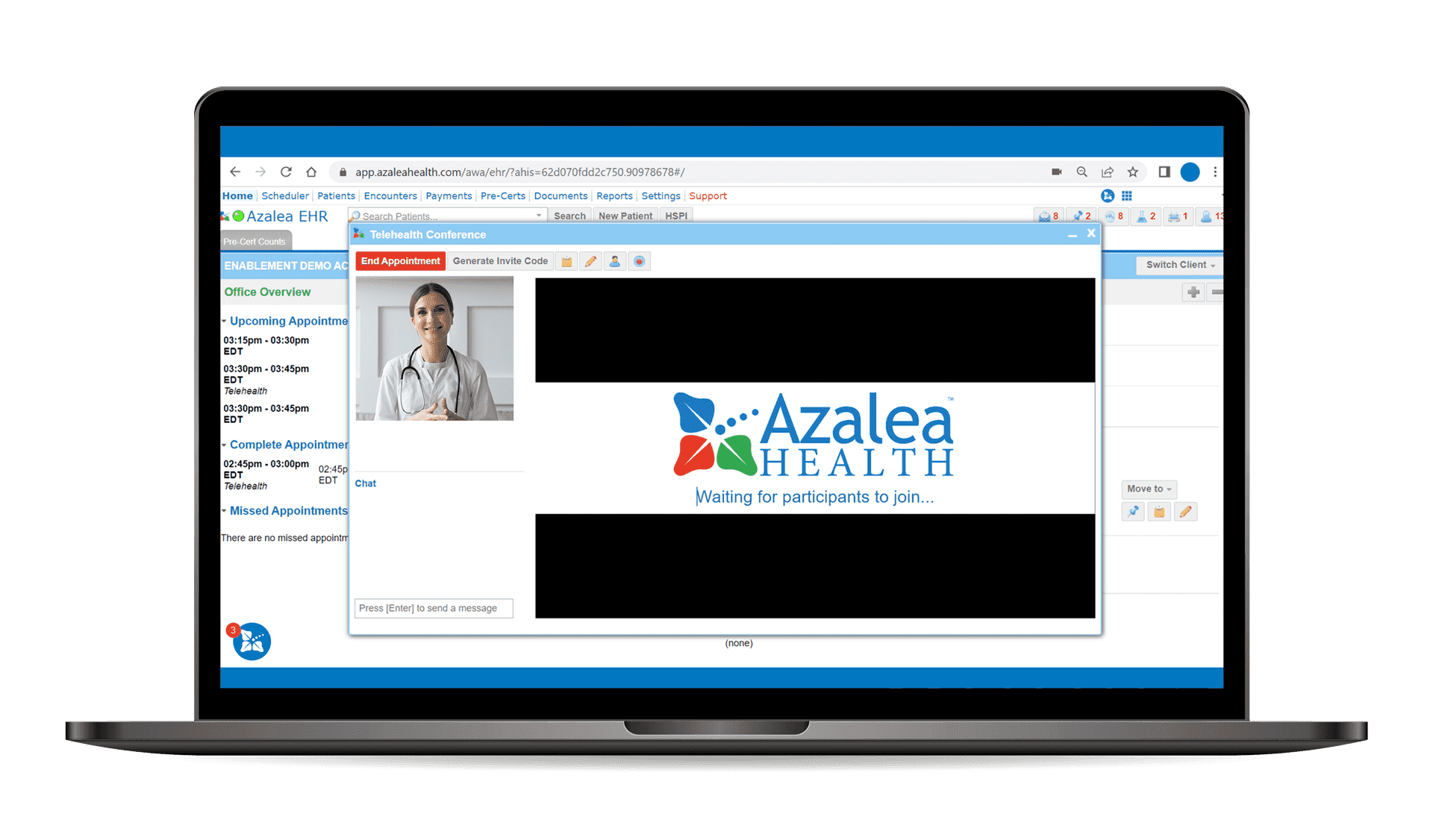
Distance shouldn’t be a barrier to care. With telehealth, it isn’t. Our telehealth solution seamlessly integrates into our platform to power meaningful connections to patients—no matter where they are.
Learn More
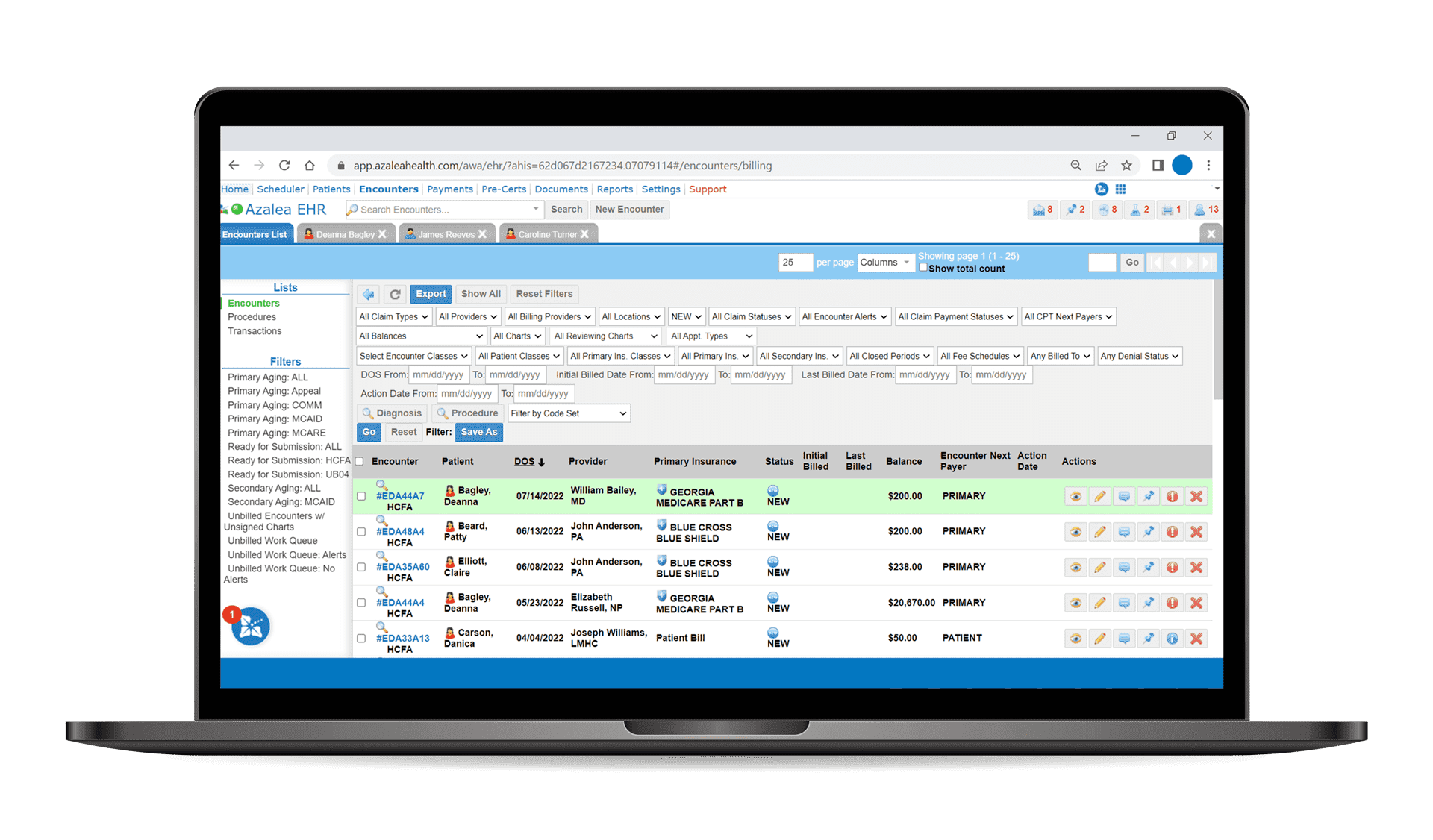
Azalea Health started as a billing company so we know how essential it is to post payments quickly and get claims out the door. Azalea Health’s Practice Management and RCM software was built to accelerate those processes, including posting payments nearly one minute faster than the industry average.
Learn More
Why Choose Azalea Health?
-
 One platform
One platform
-
 One patient,
One patient,
one record -
 One simplified
One simplified
user experience
With a single, easily-accessible platform designed to unify the clinical, financial, and operational sides of care, we can help create a seamless patient journey by making it more efficient for all involved.
While others focus solely on business intelligence, we champion provider intelligence. Our platform is purpose-built to create one record of truth—enabling a wealth of knowledge to empower a wealth of care.
By reducing the effort spent charting throughout all care settings, providers experience a more balanced work-life—more time spent with patients, reduced administrative tasks, and less time working from home.
Testimonials
Dilip Niranjana Jay, IT Admin Lead at L.A. Downtown Medical Center
“Azalea EHR, which has delivered the scalability and flexibility to support our growth and clinical quality excellence. This growth has included a 24% increase in revenue, a 25% increase in beds and a 77% increase in patient volumes within a year”
Mindy Hinkie, Revenue Cycle Director at Madison Parish
“I would recommend the clinic package to anybody. They’re able to build things the way you want them, and you’ll quickly realize it’s the best decision you can make in a rural health setting.”
Brian Miller, CEO of DeWitt Hospital
“Azalea simplified the process and worked to ensure integration into our existing radiology and lab solutions. They worked across our groups, including nursing, registration and IT, to make sure everyone was aligned, informed and prepared on Day One.”
Mindy Monroe Director of RCM at Madison Parish
“I would recommend the clinic package to anybody,” Monroe said. “They’re able to build things the way you want them, and you’ll quickly realize it’s the best decision you can make in a rural health setting.”
Kyle Parks
“Honestly, what I like tremendously about the web-based [EMR] is that while I’m here at the conference, if I need to do chart work or look up a patient it is very easy to do.”
Sandy Majors ER Hospital Group
“The hospitals I work with really value customer service – we work on it daily with our patients. So it is refreshing to find an organization that has the same value as we do.”
Questions?
We’d love to share with you how our cloud-based healthcare software can boost your ability to provide care and support the needs of your clinic or hospital.